Supporting Veterans’ Mental Health: Real Paths to Healing
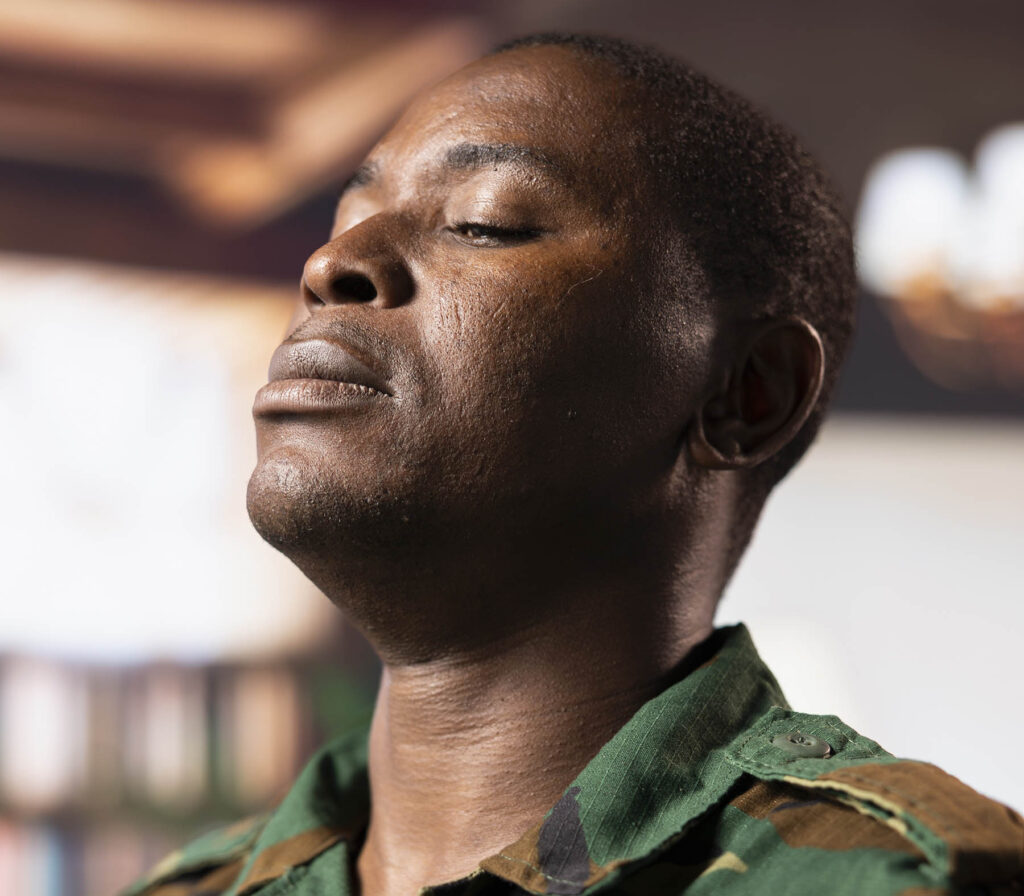
For many veterans, the hardest part of service begins after coming home. Leaving the structure, purpose, and camaraderie of military life can be incredibly disorienting. It’s not just the change in daily routine. There’s a lot of emotional weight that can come with memories, trauma, and the attempt to adjust back into normal life.
Each day, an average of more than 17 veterans die by suicide. The most recent data from 2022 shows that 6,407 veterans lost their lives this way in that year alone. These numbers reflect deep, ongoing challenges with mental health that many veterans face quietly, often without feeling seen or understood.
At Keta Medical Center, we meet veterans who have carried their invisible wounds for years. Some have tried multiple therapies or medications without success. Others are hesitant to open up at all, or they just don’t know how. The good news is that new treatments are making a real difference, offering actual relief and more personalized options for healing.
Why Mental Health Support for Veterans Matters
Many veterans live with the long-term effects of trauma, often in the form of post-traumatic stress disorder (PTSD). PTSD is a trauma-related condition that can also lead to other mental health challenges like depression, anxiety, and substance use disorders. According to the U.S. Department of Veterans Affairs, from 2001 to 2022, suicide rates among veterans receiving care for PTSD decreased by over 30%, highlighting the importance of specialized treatment.
PTSD can show up in many ways: Nightmares, flashbacks, irritability, emotional numbness, or difficulty concentrating are just a few. It can disrupt relationships, daily functioning, and even the body’s ability to regulate basic responses like sleep and appetite. For some veterans, these symptoms appear months or even years after the original traumatic event itself.
The effects of PTSD are frequently misinterpreted or overlooked, delaying the care that’s needed most. While talk therapy and antidepressants are standard first-line treatments, studies show that only about 38% of PTSD patients find adequate relief through psychiatric medications, and up to 60% continue to experience symptoms even after treatment. These numbers make it clear that many veterans need more effective options, especially when symptoms are persistent or return after initial progress.
Ketamine Treatment: A New Path When Others Haven’t Worked
Ketamine is one of the most promising new options for treatment-resistant depression and PTSD. Administered either as an intravenous infusion for PTSD or as Spravato nasal spray for treatment-resistant depression, it offers fast-acting relief for people who haven’t responded to other forms of care.
A 2024 study from the University of Michigan followed 215 veterans who had tried multiple treatments without success. After six weeks of IV ketamine infusions, nearly half showed significant improvement in depression symptoms. About one-quarter had their depression severity cut in half, and 15% entered remission. Many of these veterans also had PTSD or anxiety, underscoring the therapy’s value for those with multiple mental health challenges.
Unlike standard antidepressants, which can take weeks to show effects, ketamine often begins working within hours or days. For veterans who have spent years waiting for something to help, that speed matters. At Keta Medical Center, treatments are always guided by experienced medical staff in a safe, supportive environment.
PRISM: Another Groundbreaking Option for PTSD
For veterans living with PTSD, whether they are experiencing anxiety, sleep disturbances, flashbacks, or emotional detachment, our new PRISM offers an innovative and noninvasive treatment option. PRISM is the first FDA-approved treatment of its kind for PTSD.
What makes PRISM different is that it doesn’t require medication or revisiting traumatic memories. Instead, patients learn to calm their stress response by seeing real-time neuro feedback from their own brain activity in a computer simulation. A headset is used to monitor brain activity (through EEG, or electroencephalography). Over 15 guided sessions, patients build new, healthier patterns of response. In a recent multi-site clinical study, 67% of participants reported a significant reduction in PTSD symptoms, and 32% reached full remission.
Many veterans find PRISM especially appealing because it is noninvasive, empowering, and medication-free. It’s ideal for those who haven’t gotten the relief they need from talk therapy or medications or who simply want to try something new.
At Keta Medical Center: Compassionate Care by Medical Professionals
Every veteran’s experience is different. Some carry visible scars and others carry invisible ones. Whether you’re struggling with anxiety, depression, PTSD, or just a sense that something isn’t right, you deserve to get the help you need to heal.
At Keta Medical Center, we combine the best of science with compassionate care. Our treatments are designed both for immediate relief and long-term healing. We’re here to support you as you move forward at your own pace, with treatments that are safe, adjusted to your personal healing journey, and grounded in real-world results. Together, we’ll help you determine whether ketamine therapy, PRISM, or a combination of both is right for you.
If you or someone you know is a veteran struggling with mental health challenges, don’t wait. Explore how PRISM and ketamine therapy can offer a new path to healing. Contact Keta Medical Center today to learn more and schedule a free consultation.